
A Composite of "Why Breastmilk is Not Just Food" posts on Lakeshore Medical Clinic's Facebook Page
Jenny Thomas, MD, MPH, IBCLC, FAAP, FABM
More posts on the Facebook page frequently (ideally) that I will keep adding to this page. Dr. jen.
_________________________________________________________________________________________________________________________________

_______________________________________________________________________________________________________________________________
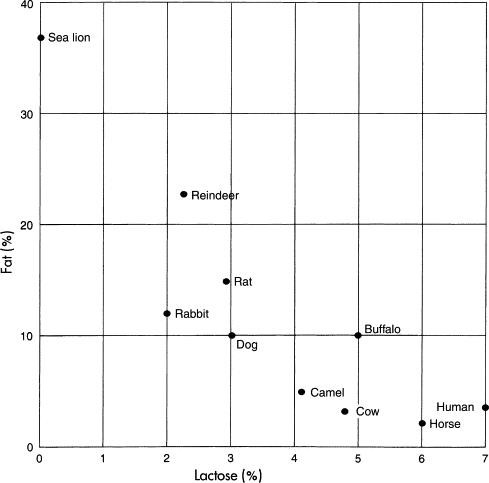
Human milk contains lactose, made by the lactating breast. Lactose is very
important for newborn growth: it enhances calcium absorption, and is helps with
the formation of lipids crucial for brain development. The levels of lactose are
consistent over the day and is important in controlling milk volume.
The graph shows the percent of lactose and fat in the milk of difference
species.
There is a correlation between the percentage of lactose in the milk and the
overall size of the brain for that species. And since lactose is a sugar found
in high concentrations in human milk, it is incredibly rare (not to mention bad
for the
species) to have an infant who is lactose intolerant. It also calls into
question the need for lactose- free or reduced lactose formulas. Image: From
Kretchmer N: Lactose and lactase, Sci Am 227:73, 1972. Copyright ©1972
________________________________________________________________________________________________________________________
Colostrum is human milk; it's just a different recipe. The term "colostrum" is not meant to mean a specific time in lactation. It is human milk that has higher concentrations of sodium, chloride, and immune substances like secretory IgA and lactoferrin, very little lactose and no casein. The changes in human milk that occur over time can be seen as a continuum. Human milk doesn't "come in." It's there changing with the changing needs of the baby.
_________________________________________________________________________________________________________________________________

This is a picture I made myself to illustrate the concept of the plasma:milk barrier. I need it for my next post. Human milk is made by a layer of epithelial cells. They are the strip of cells in the middle. They are a continuous layer of cells that get folded to make milk ducts a alveoli. During lactation these cells have to separate two very different types of fluid with very different compositions: milk and plasma. These epithelial cells need to be tightly connected to maintain this separation of fluids. And they are, by structures called, conveniently enough, "tight junctions". During pregnancy, mastitis, and weaning the tight junctions are leaky. When the tight junctions work, there is more milk volume. When they are leaky, there is less. Milk secretion and tight junctions are regulated by the body together.
________________________________________________________________________________________________________________________________

In this picture, we are concerned (today) with pathway V, the paracellular
pathway and TJ, the tight junction. During pregnancy, the TJ is leaky, so leaky
it will allow passage of large molecules like albumin and Immunoglobulin G
across the mammary epithelium. Also during pregnancy, sodium and chloride can
freely pass into the alveolar lumen through the paracellular pathway.
Then within days of
birth, tight junction close and become impermeable. As you might expect, sodium
and chloride levels in the milk drop because that pathway is no longer
available. Progesterone, the hormone that keeps milk from being secreted during
pregnancy, drops quickly in the first days after birth because of the removal of
the placenta, the main source of its production. Progesterone inhibits tight
junction closure. Glucocorticoids, necessary for milk secretion, are secreted at
birth by both the baby's adrenal glands and by the mother. Glucocorticoids close
tight junctions. Prolactin, in addition to its other numerous responsibilities,
is required to keep tight junctions closed. So, tight junctions permeable = less
milk secretion and salty milk. Tight junctions closed and impermeable = copious
milk secretion with low sodium content.
Interestingly, the milk produced during mastitis has higher levels of sodium and
chloride and potentially less milk secretion. And during mastitis, tight
junctions are leaky.
http://mammary.nih.gov/reviews/lactation/Neville001/
http://www.ncbi.nlm.nih.gov/pubmed/10819511
_________________________________________________________________________________________________________________________________

My illustration of my long post yesterday about control of milk composition and
volume through mammary epithelial cell tight junctions.
Breast epithelial cells have many roles. One is to control what gets into milk
and what stays out. Part of that process is controlled by how leaky the tight
junctions between the cells are. Leaky tight junctions let big molecules through,
and lots of sodium and chloride across without a fight, but they don't allow
much milk production. Closed tight junctions don't let anything through that
isn't invited and allows lots of milk to be made.
Tight junctions are leaky in the presence of progesterone, as in pregnancy, and
during periods of inflammation and injury, like mastitis. In pregnancy and
mastitis and around progesterone the milk is salty and low in volume.
Tight junctions are closed because of prolactin, glucocorticoids (like
adrenaline). They start to close shortly after birth and take a few days to do
so because progesterone is slowly leaving the body. That takes about 4 days or
so. The milk made when the tight junctions are closed has the composition of the
picture I have of the plasma:milk barrier I posted a few days ago.
As progesterone leaves the body, milk composition changes. This recipe is
colostrum. Still with big molecules able to cross, less sodium, and gradually
increasing volume.
_______________________________________________________________________________________________________________________________

The milk produced by mothers who have been lactating for longer than 1 year is
high in fat content and provides significant energy for the growing toddler. The
graph shows the percentage of fat (measured as creamatocrit) the duration of
lactation (in months). The child may not be getting as much breastmilk after a
year of lactation, but what they do receive packs an energy punch, like a mini
power bar.
http://
_______________________________________________________________________________________________________________________________
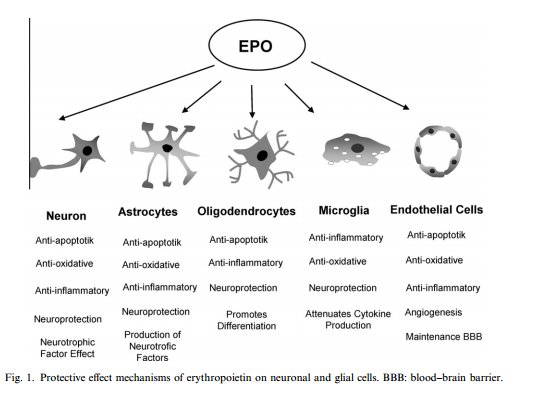
Erythropoietin is a hormone made by the kidney that is involved in the
production of red blood cells in response to hypoxia (lack of oxygen). Right?
That’s what I memorized in all those classes anyway.
But it’s also a growth hormone found in human milk and is produced by the breast
epithelium. Erythropoietin human milk may have a role in protection of the gut
and brain, aid the immune system. Concentrations
of human milk erythropoietin rise during the first months of lactation.
It has been shown to have a role in maintain “tight junctions” between cells;
maintaining barriers such as the blood:brain barrier and stopping the leakiness
of the gut by closing the endothelial cell- to- cell spaces. In the gut,
erythropoietin keeps tight junctions functional to prevent diseases like
neonatal necrotizing enterocolitis.
In the brain, in addition to maintaining the tight junctions of the blood:brain
barrier, it has been shown to have many protective mechanisms by which it
protects the neonatal brain from hypoxic injury. It works on neurons, astrocytes,
oligodendrites, and microglia in the brain (as shown in the picture).
As part of the immune system, it may protect against mother-to
child-transmission of HIV as the risk of transmission goes down with a higher
breast milk erythropoietin concentration.
The gut, the brain, the immune system: Human milk is not just food.
http://www.jbc.org/
________________________________________________________________________________________________________________________________
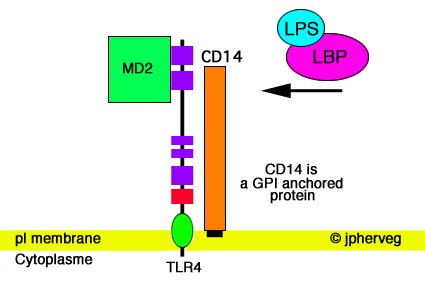
Human milk, as we have been talking about, is a crucial step in the foundation
of a healthy immune system. Part of the immune system's job is to recognize
pathogens. This starts with antigen presenting cells.
The initial recognition of the pathogens is done by Toll-like Receptors (TLR)
that are found on the antigen presenting cells. We are interested in TLR4
because TLR4 recognizes lipopolysaccharide
(LPS), a nasty lipid found on the outer membrane of gram-negative bacteria like
E.Coli that can lead to septic shock.
Human milk up regulates the production of TLR4 so that in presence of CD14
(cluster of differentiation 14) and MD-2 will bind gram negative aerobic
bacteria like E.Coli. This CD14 is found in abundance in early human milk in a
soluble form (sCD14). So, human milk contains both TLR4 and sCD14 in abundance
early in life.
sCD14 also helps in the gut. Combined with alpha-lactalbumin (the same protein
as we discussed in HAMLET cells) the sCD14 is allowed to continue farther down
the GI tract than it could alone. This complex of sCD14 and alpha-lactalbumin is
only around very early after birth suggesting a role for it in coordinating
early good microbe colonization of the gut in a very small, important, window of
time.
The TLR effect is present only during the first 5 days of life . Up or down
regulation of transcription of genes is controlled by human milk on an hour by
hour basis . Any alteration in HM or addition of formula interferes with TLR
regulation.
Have a good reason to supplement. Human milk is more than just food.
http://basic.shsmu.edu.cn/
________________________________________________________________________________________________________________________________
__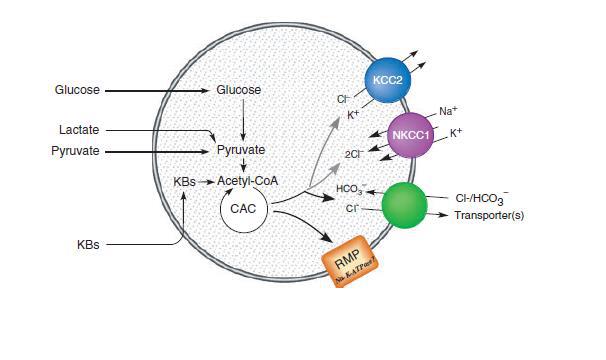
After birth, the nutrient flow the baby received through the placenta is
interrupted allowing maternal metabolism to transition to lactation. Glucose is
the main source of energy for the brain. However, immediately after birth and
before the onset of suckling there is a time in which the newborn undergoes a
unique kind of "starvation" where glucose is scarce. This normal and expected.
The energy balance is eventually regained through human milk nutrients which
supply the newborn with ketone bodies required for energy. However, during this
short period of "starvation" and scarce glucose, ketone bodies are also not
available because of a delay in ketogenesis. Fortunately, the newborn is
supplied with other metabolic fuels, lactate and pyruvate, which are then used
as the source of energy for the neonatal brain. The picture shows the possible
effects of these energy substrates on neonatal neuron. The neonatal brain can
use not only glucose, but lactate, pyruvate and, ketone bodies (KBs). These
substrates are then converted into acetyl-coenzyme A, the main input for the
citric acid (Krebs) cycle leading to ATP (energy production). Glucose alone,
even at high concentration, cannot maintain mitochondrial respiration at the
level necessary for optimal neuronal functioning. Complementing glucose with
pyruvate, lactate or ketone bodies allows energy demands to be met. This results
in normal neuronal functioning, in a stimulation of pumps, transporters or
channels (the colored circles on the picture) allowing the neonatal brain to
survive a period of low glucose with no damage to the function of the neurons.
This ability of the newborn to use ketone bodies as a source of energy has
consequences outside the brain. During the early postnatal period, the ketones
acetoacetate and beta-hydroxybutyrate are used instead of glucose as substrates
for creation of phospholipids used in brain myelination. In the lung,
acetoacetate works better than glucose as a precursor for the synthesis of lung
phospholipids. The synthesized lipids are incorporated into surfactant, and may
therefore have a role in maintaining lung function during the early days of
life.
This dip in glucose after birth is normal and turns on a cascade of important
other events in development. We should have a very good reason to interrupt
these important physiologic changes. Human milk is more than just food.
image
http://www.ncbi.nlm.nih.gov/pubmed/3884391
http://www.ncbi.nlm.nih.gov/pubmed/3884392
________________________________________________________________________________________________________________________________
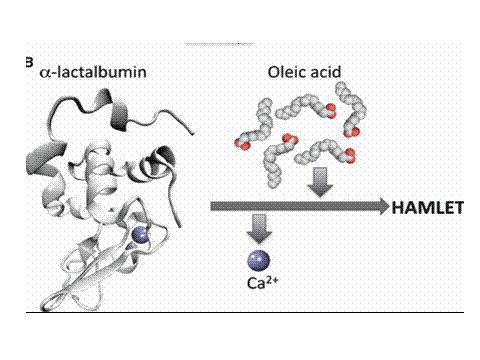
Proteins have a shape, "the native fold," that has traditionally been seen as
its only relevant functional state. But, research done over the the past decade
shows that partial unfolding that native fold allows common proteins to adopt
new, physiologically relevant functions. Human milk contains α-lactalbumin,
which by unfolding can form a tumoricidal complex with oleic acid creating a
complex called Human α-lactalbumin Made Lethal to Tumor cells (HAMLET). It can
kill tumor cells and has documented therapeutic use.
Human α-lactalbumin is a globular milk protein, expressed in secretory cells of
the lactating mammary gland during the whole lactating period. Alpha lactalbumin
undergoes transformations in the cell and becomes important in lactose
production. The α-lactalbumin gene comes from an ancestral lysozyme gene. (Shown
in the picture from yesterday talking about embryology of the mammary gland.)
With removal of calcium from alpha-lactalbumin, under the right conditions, it
can bind with fatty acids. When it binds with oleic acid, it becomes HAMLET.
HAMLET is taken in by tumor cells, targets distinct cellular organelles and
activates several cell death pathways.
http://www.ncbi.nlm.nih.gov/pubmed/20977665
________________________________________________________________________________________________________________________________


These graphs shows that exclusive human milk reduces gut permeability but
not right away. The gut of exclusively breastfed infants is "leaky" in the first
few days. And since breastfeeding is normal, this increased permeability is
normal.
Molecules
may penetrate freely into the bloodstream before day 7.
The leakiness also helps the immune system, the development of which is delayed
in most species.
And maybe this delay doesn't make sense. Why wouldn't we want to have an intact
immune system to fight pathogens? First, We have protections in the newborn gut
that make this leakiness make sense. The defenses in a newborn gut are
constructed to make sure there is no inflammation when responding to invaders.
And some "invaders" are good bacteria needed to start the immune system off
right.
Human milk simulates the strictly held balance of immune cells that are crucial
for developing an immune system that recognizes what to get rid of and what to
keep, what to destroy and what to leave alone.
And the delay allows for less energy and nutrients to be used for the immune
system of the infant. That's good because, when the immune system does need to
work, the processes needed increase nutritional and energy demands. That extra
energy can then be used for the growth and development of the CNS and lung.
This all works because of human milk. All the defenses given to the infant from
human milk (antimicrobial, antiinflammatory, and immunomodulating agents)
protect from inflammation. Plus, it just makes sense and is really efficient
that most of the antimicrobial and other defense agents in human milk are used
to nurture the baby. Not fight battles.
You guessed it. Human milk is more than just food.
http://journals.lww.com/
________________________________________________________________________________________________________________________________
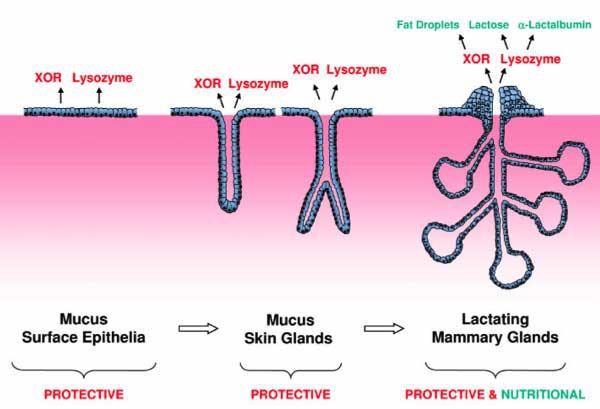
What if the mammary gland was not initially meant to provide nutrition but
developed, at first, to be part of the innate immune system? The innate immune
system is a rapid, generalized defense system (which I have compared to Clay
Matthews in the past, with apologies to those who don't understand American
football) and is run by small peptides and T-cells. The innate immune system is
different from the acquired immune system, which is predominantly
immunoglobulins and is very specific (like a really good cornerback, like
Charles Woodson).
In embryology, skin glands with protective infection-fighting effects are very
common. The mammary gland evolved from a mucus-secreting skin gland, which would
then help protect the skin of the newborn, even if the "newborn" was an egg.
Mucous secretion contains many things we've already talked about: lactoferrin,
IgA and others I haven't posted about yet like xanthine oxidoreductase (XOR) and
lysozyme. Those same protective skin mucus secretions are also found in the
mammary cells.
XOR, as well as being an important part of the innate immune system is also
crucial in milk fat droplet secretion. Lysozyme is an anti-microbial but also
evolved into alpha -lactalbumin, a nutritional whey protein special to the
lactating breast. So both have two roles- one protective, one nutritional. For
both though, their immune system function came first.
So, the mammary gland went from an immune system gland to a protective and
nutritional gland --one that is unique to mammals. Breastmilk is more than just
food.
http://capecchi.genetics.utah.edu/PDFs/150Vorbach.pdf
_______________________________________________________________________________________________________________________________
____________________________________________________________________________________________________________________________

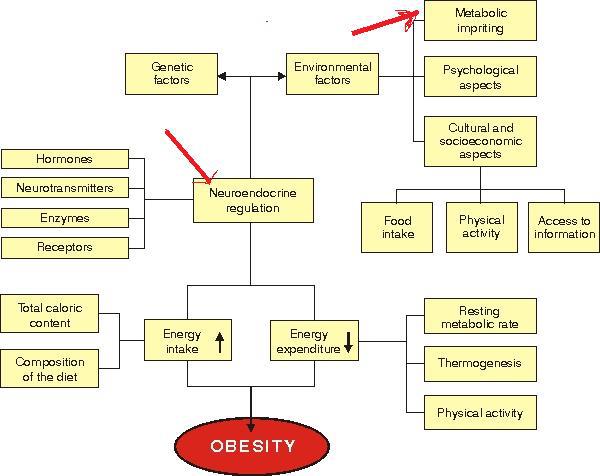
Human milk contains regulatory hormones that control food intake and glucose and
lipid metabolism. Among these are adiponectin, and leptin. Adiponectin is a
hormone produced by fat cells. It plays a role in the regulation of glucose
metabolism, and increases insulin sensitivity. (Insulin increases the effects of
prolactin and is also required to make human milk.)
Leptin is a hormone that can be transferred into human milk from maternal serum
and is also made by the lactating breast. It decreases food intake. Fully
breast-fed infants have higher serum levels of leptin than formula-fed infants.
Both adiponectin and leptin are found throughout the duration of breastfeeding.
The graph shows that higher breast milk leptin levels during the first week
after birth are correlated with lower infant weight gain from the end of the
first week to the sixth month.
This first week is a critical period where the baby changes from a placental to
an oral energy and nutrient supply and is "programmed." These hormones are
likely factors that influence babies in a critical developmental period and help
determine the risk of diseases later in adulthood. We should have a really good
reason for interrupting this programming with something other than human milk
because...breastmilk is more than just food.
http://www.ncbi.nlm.nih.gov/pubmed/21857386
http://www.ncbi.nlm.nih.gov/pubmed/21407103
_____________________________________________________________________________________________________________________________
Human milk contain Ghrelin. The "gh" represent "growth hormone" as one of its
functions is to stimulate growth hormone secretion. It also stimulates release
of other pituitary hormones such as adrenocorticotropin (ACTH) and prolactin
(both of which are required to make human milk).
Ghrelin increases appetite. Endogenous ghrelin levels get higher when not eating
and fall after eating, showing that
this peptide acts as a short-term regulator in energy balance. On the other
hand, leptin, which I posted about yesterday, does the opposite: it decreases
acutely after fasting, generally acts as a long-term peptide, and decreases
appetite.
Ghrelin may independently regulate energy balance acting opposite of leptin
using growth hormone (GH) secretion (and other mechanisms). It helps with short-
term energy imbalance. These regulating hormones, leptin, adiponectin, ghrelin,
and adipocyte fatty acid binding protein are found in human milk and are
considered to influence nutritional status and possibly play a role in the
development or prevention of obesity. Human milk is more than just food.
http://onlinelibrary.wiley.com/doi/10.1111/j.1651-2227.2005.tb01934.x/full
_____________________________________________________________________________________________________________________________
 ______________________________________________________________________________________________________________
______________________________________________________________________________________________________________
The previous post talks about regulatory hormones involved with obesity. It
specifically addresses adiponectin and leptin but other hormones such as ghrelin,
and adipocyte fatty acid binding protein are found in human milk and are
considered to influence nutritional status and possibly play a role in the
development of components of metabolic syndrome later in adulthood. Human milk
plays a role in the prevention of obesity. I even put arrows on the photo to
highlight that breastmilk is more than just food. (Image from
http://www.jped.com.br/
_____________________________________________________________________________________________________________________________
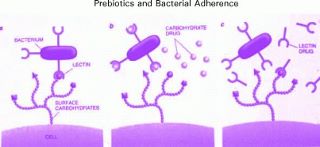
Human milk contains prebiotics. This cartoon shows how *prebiotics* (not
probiotics) in human milk work: They are non-digestible food components that
beneficially affect the gut by providing food for the good bacteria that
(hopefully) already inhabit it. In human milk, the most common prebiotics are
oligosaccharides, which are also the third most common component of mature human
milk. The
picture
shows the ways in which prebiotics work. The non-pathogenic bacteria (the good
ones) can bind to the cell surface because of they contain the right receptors
to let them bind (far left part of the slide).
The virulence of most pathogenic microorganisms, for example, Campylobacter
jejuni, Escherichia coli, Vibrio cholera, and Shigella and Salmonella strains,
often depends on their ability to adhere to the gut's epithelial surface.
Pathological bacteria are inhibited from attaching either because a prebiotic
has plugged the part of the bacteria that helps it attach (middle picture) or
blocks the receptor site (third picture).
That means that the body can respond to pathogenic bacteria without inflammation
because the pathologic bacteria never had a chance to attach and cause damage.
This need to prevent inflammation is one of the reasons there is such an
abundance of oligosaccharides in human milk.
And as an abundant, non-digestible component of human milk, oligosaccharides
help with frequent stooling, preventing constipation and aiding in the removal
of bilirubin. Human milk is more that just food.
http://www.ncbi.nlm.nih.gov/pubmed/15877894
___________________________________________________________________________________________________________________________
Human milk contains beta- endorphins (endorphin meaning "endogenous morphine") that function like opioids because they produce analgesia and a feeling of well-being. The concentration of beta-endorphins in colostrum the fourth postpartum day of mothers whose babies who were born vaginally, at term, or prematurely were significantly higher than colostrum levels who had a cesarean section. The highest levels were found in mothers who had delivered vaginally and preterm, a difference which lasted until the transitional milk phase (10th day). Those differences were gone in mature milk (30 days). These differences may show a role of beta- endorphins in postnatal fetal adaptation, overcoming birth stress of natural labor and delivery. Our bodies taking care of our babies, helping with pain. Isn't human milk so much more than just food? http://www.ncbi.nlm.nih.gov/pubmed/11568517 http://www.ncbi.nlm.nih.gov/pubmed/11223648
___________________________________________________________________________________________________________________________
Human milk contains two main types of proteins: whey and casein. The casein fraction contains multiple sub-types, two of which are kappa and beta caseins. Kappa casein is an anti-adhesive. It inhibits the binding of H. pylori to the gastric lining and Strep pneumo and H. flu to the respiratory epithelium. Kappa casein is an opioid antagonist, working against the effects of opiods in the gut and elsewhere. Conversely, human milk contains beta casein which is responsible for the production of beta casomorphin. Beta casomorphin is a peptide with opiate-like properties which is absorbed through the gastrointestinal mucosa. It has been shown to affect gastrointestinal motility, absorption and secretion and has been postulated to have a role in the development of the immune system. The relative proportion of the beta- and kappa-casein subunits varies throughout lactation, meeting the needs of the growing child. Breastmilk is more than just food. It's got opioids in it! http://www.ncbi.nlm.nih.gov/pubmed/2358977 http://www.ncbi.nlm.nih.gov/pubmed/2760302 __________________________________________________________________________________________________

The above graph represents the whey to casein ratio during lactation as
explained below. The figure is from
http://
____________________________________________________________________________________________________________
Human milk contains vitamin B12 binding protein in large amounts. E.coli and Bacteroides bacteria use vitamin B12 for growth. Both can cause serious infections, especially in newborns. This binding protein is just another example of the infection-fighting properties of human milk and another cool reminder that breastmilk is not just food.
_______________________________________________________________________________________________________________
Human milk contains Lactoferrin, a protein with many responsibilities. It binds iron, which prevents certain bacteria from growing in breastmilk and in mucosal secretions. It is bactericidal, preventing E. Coli from attaching to the gut wall and Shigella from invading into the body. It is an anti-viral, preventing viruses from attaching or invading. It is an anti-inflammatory, decreasing cytokine release. And it affects neonatal intestinal growth and recovery from injury, thereby helping to prevent infection. Breastmilk is more than just food.
______________________________________________________________________________________________________________
During fetal development, the breast is derived from that glands were first associated with the skin. The embryonic signaling pathways that then turn cells into breast tissue involve some of the same signaling pathways that are associated with T lymphocytes. Some authors have suggested that the breast was first an immune system organ and then developed to become a source of nutrition. Breastmilk is more than just food.
______________________________________________________________________________________________________________
We already know the Prolactin is necessary for the production of breastmilk, but it is also a known component of breastmilk and made by the lactating breast. As a part of breastmilk, it exerts immunomodulating effects in the newborn when it helps with lymphoctye cell growth and function. Prolactin in milk also influences maturation of gastrointestinal epithelium. The concentration of Prolactin is highest in the first 3 days of life when it exerts crucial neuroendocrine effects. These effects condition behavior responses in later life. Breastmilk is not just food
______________________________________________________________________________________________________________
Human milk has been recently found to contain microRNA, molecules involved in the control of the development and function of Regulatory T cells. Among other roles, Regulatory T cells are crucial for preventing autoimmune diseases and limiting chronic inflammatory diseases. These microRNA molecules are abundant in human milk and transferred from mom through breastmilk in something called an exosome: vesicles than help with intercellular communication. More evidence that breastmilk in critical to immune system development, both short and long term and...that breastmilk is more than just food.
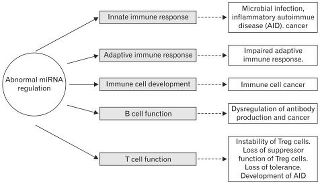 Image
from: http://
Image
from: http://
________________________________________________________________________________________________________________
We already know that human milk contains vitamin anti-oxidants like vitamins A,
E and C. Antioxidants protect cells from the damaging effects of free radicals.
In addition, proteins in human milk can prevent free radical damage. Tryptophan
is an amino acid produced from protein digestion. As human milk proteins are
digested the the neonatal gut, tryptophan is produced. Tryptophan is a powerful
free radical scavenger and enhances pathways that decreases oxidative stress in
the newborn gut. This has tremendous implications especially for premature
infants, as necrotizing enterocolitis is associated with oxidative stress. Human
milk can save lives and...breastmilk is more than just food.
And as requested by the "internet science geeks" http://
____________________________________________________________________________________________________________
This is an electron microscopic view of an enteric bacterium interacting with the microvillus surface of the small intestine, something called microbial–epithelial ‘crosstalk’. This communication represents an important stimulus to the development of host defense of the developing neonatal gut. The bacteria, the things that look like peanuts are "talking" to the lining of the gut, and those "villi" (the stringy things) look as if they are listening. This cross talk is thought to help set up the architecture of the gut. And makes it even more important that the right bacteria are doing the talking. The gut is the second biggest organ of the immune system, right behind skin. Getting it right from the start is very important for a healthy immune system. Breastmilk is more than just food.
 Image
and info from: http://
Image
and info from: http://
____________________________________________________________________________________________________________
Human milk contains the enzyme platelet-activating factor acetylhydrolase. It is
released from human milk macrophages. This enzyme turns one of the most potent
pro-inflammatory agents so far described, platelet activating factor, into a
form which has no physiologic activity. Platelet activating factor causes GI
tract ulcers and causes the development of necrotizing enterocolitis within
hours after administration to experimental animals. Therefore
platelet-activating factor acetylhydrolase protects the intestine of the newborn
from inflammatory disease and much worse. Breastmilk is so much more than just
food.
more info for my nerds... http://
_____________________________________________________________________________________________________
Human milk contains both pro-inflammatory and anti-inflammatory components. It
contains Interleukin which is group of cytokines. Cytokines are secreted
signaling proteins that facilitate communication among cells. Although we know
that interleukins are present in human milk, their function isn't always known.
That's not true for Interleukin 7 (IL-7). IL-7 has been linked directly with
increased output of the thymus, a critical organ in the development of T cells,
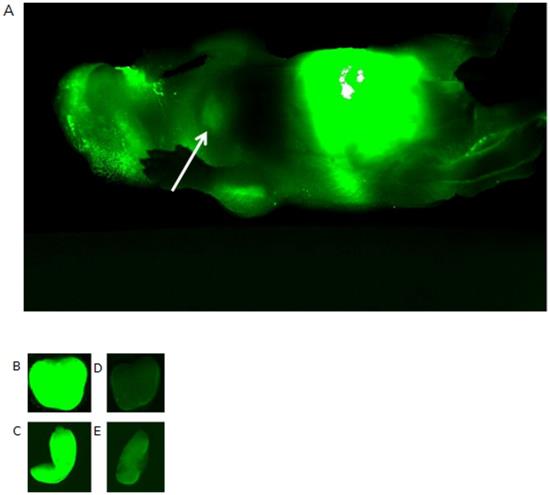
and therefore the adaptive immune system. This photo is of a mouse given
recombinant IL-7 labeled with a fluorescent dye to trace the movement of IL-7
from the stomach across the gut and into the lymphoid tissues. The arrow shows
green fluorescence in the anterior mediastinum, where the thymus is found, on
the next day. Other photos B,C,D, E show the thymus and spleen of mice given
albumin (as a control) or IL-7. The two pictures of the IL-7 mice (B,C) show
more uptake, showing again that IL-7 directly increases T cell production in the
thymus and supports the survival of T cells in the peripheral secondary lymphoid
tissue (like the spleen). More IL-7, more T cell maturation, bigger thymus. Have
I mentioned, breastmilk is more than just food?
The mouse head is on the left, tail on the right. The belly is bright green, the
arrow shows the thymus. Geek alert:
http://www.plosone.org/
__________________________________________________________________________________________________________________

In the "just one bottle article" and in the post above I said the thymus of breastfed kids can be twice the size of those who are not. Here's a good picture showing how large it can get. The thymus helps the development of T cells, important cells of the immune system, and requires colostrum to get that process started. Image from From: Nasseri F , Eftekhari F Radiographics 2010;30:413-428
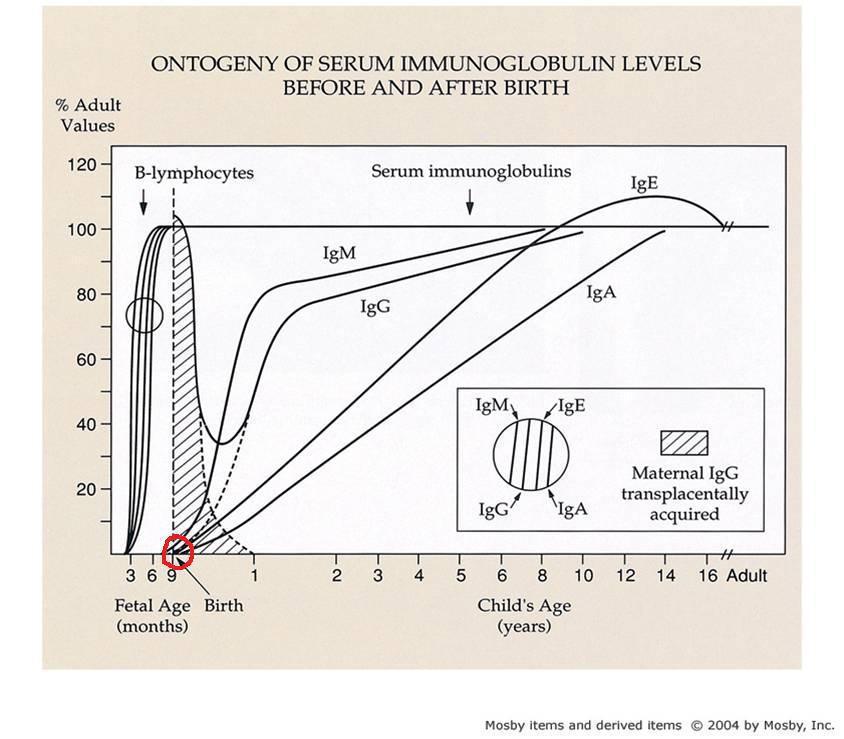
I circled in red the starting point of the immune system in a newborn. The graph
shows that the infant's immune system relies on maternal IgG that crosses the
placenta but is otherwise pretty empty in the first week of life. (IgG
antibodies are very important in fighting bacterial and viral infections.) So,
the first week of life represents a sensitive window of opportunity to program
the immune system.
If you follow the lines, IgM, IgE and IgA are almost at nothing at birth. IgA
antibodies protect body surfaces that are exposed to outside foreign substances.
It's "sticky" and love places like the respiratory tract, gut, nose, even eyes.
IgM is usually the first to be produced in an infection. It also causes other
immune system cells to destroy foreign substances. IgE is most often associated
with allergies, but can help fight fungi and parasites. And none of them are
there at birth.
So, the first week of life represents a sensitive window of opportunity to
program the immune system to develop tolerance, (so we don't attack ourselves)
immunity, host defense in the neonatal gut *without* inflammation (how cool!)
and immunological memory (so if the same organism attacks, we remember how to
fight it without starting from scratch).
This process starts off and absolutely needs the transfer of breastmilk. We
really, really, really need to know why we are supplementing with something
other than human milk if we are supplementing. Human milk is so much more than
food.